DENVER — The Colorado health department has updated its guidelines for hospitals in case the governor declares a public health emergency because of COVID-19.
To be clear, as of Monday, April 6, Gov. Jared Polis has not made such a declaration; however, the Colorado Department of Public Health and Environment (CDPHE) is preparing for that possibility with its plan for crisis standards of care.
"(COVID-19) could quickly overwhelm the hospital system and especially (Intensive Care Unit) beds and ventilators," Jill Hunsaker Ryan, Executive Director of CDPHE, said.
Dr. Stephen Cantrill is a Denver Health emergency physician who served in the group of experts who developed the updated recommendations. He says an umbrella policy is needed.
"This is not just about trying to fix the problems in the hospital. It's trying to fix the resource problems across the region," Cantrill said. "If I run out ventilators and I have a patient who needs a vent, there might be a vent across town."
The Crisis Standards of Care plan is designed to eliminate any implicit bias like money, race, or sexual orientation, according to Gina Febbraro, with the CDPHE Prevention Services Division.
"Talking about limited resources and the speed of which decisions are made, there's a concern that this is where some judgement and there's some fear that people won't be treated fairly and equitably," Febbraro said.
In other words, these are the guidelines that hospitals would follow to determine which patients get the beds, ventilators, etc. when there aren't enough of those things to go around.
CDPHE developed its crisis standards of care in 2018, but that plan needed to be updated for the specific challenges of COVID-19.
Eric France, CDPHE's chief medical officer, said in a virtual news conference on Monday that health officials expect 30% to 40% of Coloradans to be infected with COVID-19 over the coming months. That would be more than 2 million people.
According to projections from the American Hospital Association:
- 5% of COVID-19 patients will be hospitalized.
- 40% of those patients could be admitted to the ICU.
- 50% of ICU patients will need a ventilator.
In addition, the majority of COVID-19 patients with a serious breathing issue would need a ventilator for more than 12 days, according to the CDPHE release.
"With that kind of burden facing us, we may run the risk of having scarce health care resources to take care of our population," France said.
The updates were approved Sunday by the Governor's Expert Emergency Epidemic Response Committee.
According to the updated guidelines, every hospital should have a triage team of four members:
- An expert on ethics or palliative care, which is specialized care for those who live with a serious illness.
- An attending physician who's familiar with critical care.
- A nursing staff representative.
- A hospital leadership representative.
The triage team is activated in a crisis when a hospital approaches its capacity for resources like beds and ventilators, and will decide with a specific set of criteria how to allocate those resources.
The medical team for a patient should not be involved in triage decision-making for that patient, to make sure decisions are objective.
Also, the triage team can't base decisions on factors such as race, ethnicity, ability to pay, disability status, national origin, primary language, immigration status, sexual orientation, gender identity, HIV status, religion, veteran status, "VIP" status and criminal history.
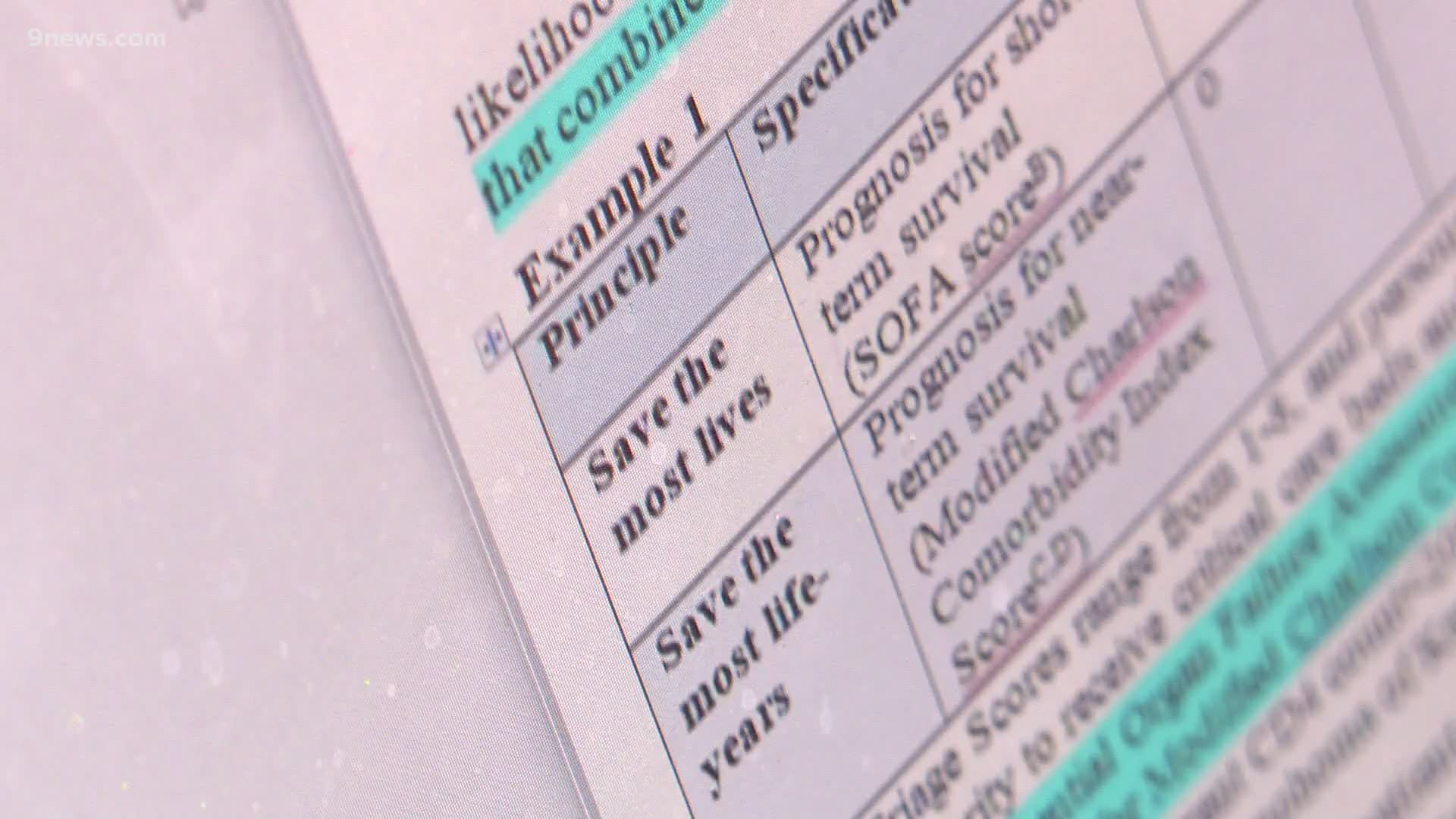
The triage team makes decisions on care based on a tier system, i.e. using the top tier as its first level of criteria, then moving down to the secondary tier in case of a tie in the top tier, and so on.
- Tier 1: A scoring system based on a combination of acute illness and the likelihood of surviving weeks, and of chronic illness and the likelihood of surviving months or years.
- Tier 2: Children, health-care workers and first responders.
- Tier 3: Special considerations such as pregnancy, life-years saved and whether the patient is a sole caregiver.
- Tier 4: Random allocation.
CDPHE has been working hard to avoid having to implement the crisis standards of care, France said in the release.
"We're working with the hospitals to increase the number of ICU beds and ventilators to try and meet the anticipated demand," France said. "We need everyone's help to slow the spread of the virus by following public health orders, to reduce the likelihood of putting these standards into place."
CDPHE also recommends that everyone sets up a living will that names a health care power of attorney and outlines the medical interventions that a person wants and doesn't want. This document, also called an advanced directive, would ensure your wishes are carried out if you can't communicate with a doctor.
RELATED: Colorado's governor wants everyone to wear face masks in public. Here's how to make your own
SUGGESTED VIDEOS | Local stories from 9NEWS